One leukemia Is a blood cancer And of the bone marrow which is characterized by excessive and uncontrolled production of abnormal white blood cells. These cancer cells gradually invade the bone marrow, disrupting the normal production of other blood cells (red blood cells, normal white blood cells, and platelets). In France, leukemias affect between 9,000 and 10,000 people each year. The median age at diagnosis varies according to the type of leukemia: chronic forms are more common in adults, especially the elderly, while acute forms can occur at any age, including children. Among those under 17 years of age, leukemias represent 26% of diagnosed cancer cases.
They appear within a few weeks or months and require rapid treatment.
Acute lymphoblastic leukemia (ALL)
→ Immature lymphocytes (lymphoblasts) become cancerous.
Acute myeloid leukaemia (AML)
→ The cells that make red blood cells, white blood cells, and platelets become abnormal. More common in adults.
Other rare acute leukemias:
They progress over several years and can sometimes be monitored without immediate treatment.
Chronic lymphocytic leukemia (CLL)
→ B cells multiply excessively without functioning properly. Especially among the elderly. Slow evolution, often detected by chance.
Chronic myelogenous leukemia (CML)
→ A genetic anomaly (Philadelphia chromosome) causes an overproduction of white blood cells. Can remain stable for a long time.
Acute lymphoblastic leukemia (ALL)
Acute myeloid leukaemia (AML)
Unlike solid cancers that use the TNM system, acute leukemias are classified according to the WHO classification. This is based on three main criteria:
1. Classification of acute lymphoblastic leukemia (ALL)
ALL affects immature lymphocytes (lymphoblasts). The WHO divides it into subtypes according to:
A. The cell line
B. Associated genetic abnormalities
Some mutations influence the treatment and evolution of the disease.
2. Classification of acute myeloid leukemia (AML)
AML affects myeloid cells (precursors of red blood cells, white blood cells and platelets). The WHO categorizes AML into four categories:
A. AML with specific genetic abnormalities
These mutations influence prognosis and response to treatment.
B. AML secondary to myelodysplastic syndrome
Occurs in patients who already have chronic blood diseases.
C. AML linked to chemotherapy or radiation therapy
Develops after cancer treatment.
D. LAM not otherwise classified
Includes rare and atypical forms.
Chronic Lymphocytic Leukemia (CLL)
Chronic myelogenous leukemia (CML)
t (9; 22) — Philadelphia chromosome (BCR-ABL1) → Translocation
1. Classification of chronic lymphocytic leukemia (CLL)
CLL affects mature B cells, which become abnormal and build up in the blood, bone marrow, and lymph nodes. The WHO classifies it according to two main criteria:
A. Associated genetic abnormalities
These mutations influence the response to treatments.
B. The specific variants of LLC
Atypical LLC → Cases that don't exactly meet the classical criteria.
Prolymphocytic leukemia (LPL) → More aggressive form with abnormal prolymphocytes.
Hairy Cell Leukemia → Rare form, affecting B lymphocytes, often well controlled by specific treatments.
2. Classification of chronic myelogenous leukemia (CML)
CML is caused by a specific genetic anomaly: the t (9; 22) translocation — Philadelphia chromosome, which merges the BCR and ABL1 genes, causing excessive production of abnormal white blood cells. The WHO divides CML into three phases according to its evolution:
A. Chronic phase (initial phase)
B. Accelerated phase
C. Blast phase (blast crisis)
Chronic leukemias progress slowly and do not always require immediate treatment. The therapeutic approach depends on the aggressiveness of the disease and the genetic abnormalities present.
Targeted therapies (reference treatment)
One targeted therapy is a drug treatment that specifically targets genetic or molecular abnormalities or alterations present in cancer cells or other diseased cells.
Unlike conventional treatments such as chemotherapy that act on all cells in the body, targeted therapies work more selectively, by blocking or inhibiting specific proteins involved in the growth and proliferation of cancer cells or in other diseases.
Targeted therapies are often used in combination with other treatments such as chemotherapy or radiation therapy. They are being used more and more in the treatment of cancer.
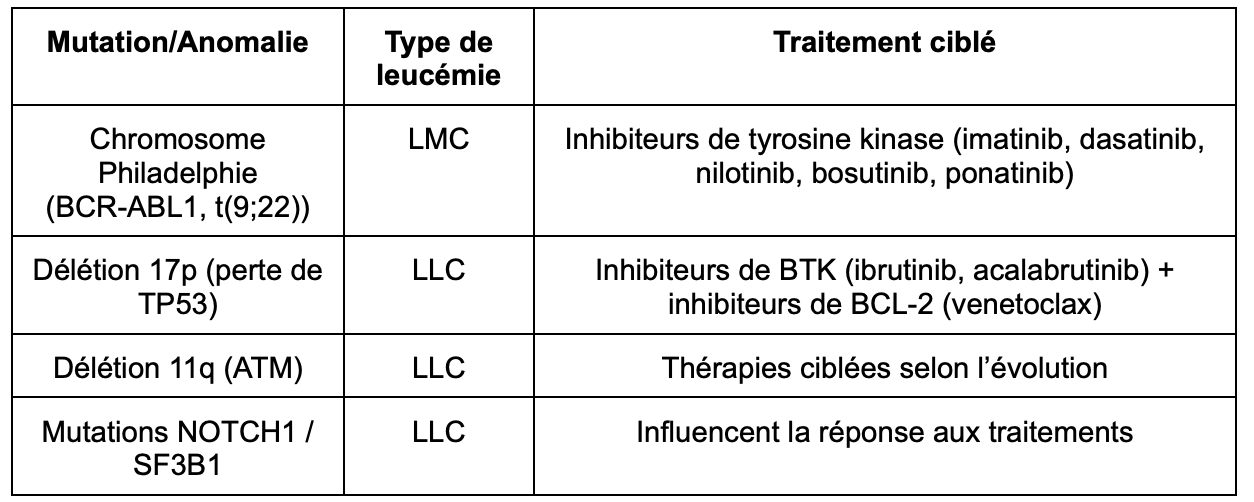
In the case of chronic leukemias, here are the most used targeted therapies:
Immunotherapy
Immunotherapy is a treatment that stimulates or changes the immune system to help fight cancer. It uses antibodies, vaccines, or other agents to enhance the body's ability to detect and destroy cancer cells. This treatment can be used alone or in combination with other treatments such as surgery, chemotherapy, or radiation therapy.
It is used for CLL to target cancer cells. The most used is the following:
Immunotherapies are often combined with targeted therapies for better efficiency.
Chemotherapy (less and less used)
Chemotherapy is a treatment that uses powerful drugs to destroy cancer cells by stopping them from multiplying or spreading in the body. Chemotherapy medications can be given intravenously (into a vein), orally (as tablets or capsules), or by subcutaneous injection (under the skin).
Chemotherapy may be used alone or in combination with other treatments such as surgery or radiation therapy, depending on the type and stage of the cancer, as well as the patient's overall health. While chemotherapy can be very effective in destroying cancer cells, it can also damage healthy cells, leading to side effects such as hair loss, fatigue, nausea and vomiting, and suppression of the immune system.
In the case of chronic lymphoid leukemias, chemotherapy is used in cases of resistance to targeted therapies or if no target mutation is identified. We find: Fludarabine, cyclophosphamide, bendamustine. It is rarely used for chronic myeloid leukemias.
Bone marrow transplant
Bone marrow transplantation is used very rarely for chronic leukemias. It is mainly used in last resort in case of resistance to standard treatments.
It is mainly indicated in Refractory LMC Or in Aggressive LLC.
How are acute leukemias treated?
The treatment of acute leukemias is based on a multi-phase approach to eliminate leukemia cells and restore normal blood cell production.
Chemotherapy (basic treatment)
Chemotherapy is a treatment that uses powerful drugs to destroy cancer cells by stopping them from multiplying or spreading in the body. Chemotherapy medications can be given intravenously (into a vein), orally (as tablets or capsules), or by subcutaneous injection (under the skin).
Chemotherapy may be used alone or in combination with other treatments such as surgery or radiation therapy, depending on the type and stage of the cancer, as well as the patient's overall health. While chemotherapy can be very effective in destroying cancer cells, it can also damage healthy cells, leading to side effects such as hair loss, fatigue, nausea and vomiting, and suppression of the immune system.
In the case of acute leukemias, the goal of chemotherapy is to destroy leukemia cells in the bone marrow and blood. It is used in all acute leukemias (ALL and AML). Among the most used chemotherapy drugs are:
Targeted therapies (treatments based on the genetics of leukemia)
One targeted therapy is a drug treatment that specifically targets genetic or molecular abnormalities or alterations present in cancer cells or other diseased cells.
Unlike conventional treatments such as chemotherapy that act on all cells in the body, targeted therapies work more selectively, by blocking or inhibiting specific proteins involved in the growth and proliferation of cancer cells or in other diseases.
Targeted therapies are often used in combination with other treatments such as chemotherapy or radiation therapy. They are being used more and more in the treatment of cancer.
In the case of acute leukemias, here are the most used targeted therapies:
Immunotherapy (stimulates the immune system against leukemia cells)
Immunotherapy is a treatment that stimulates or changes the immune system to help fight cancer. It uses antibodies, vaccines, or other agents to enhance the body's ability to detect and destroy cancer cells. This treatment can be used alone or in combination with other treatments such as surgery, chemotherapy, or radiation therapy.
It is used for LAL, especially if chemotherapy treatment is unsuccessful. Among the immunotherapies used, we find:
Monoclonal antibodies
CAR-T therapy (laboratory modified T cells)
Bone marrow transplant (hematopoietic stem cell transplantation)
The aim of bone marrow transplantation is to replace diseased bone marrow with healthy marrow. It is used in case of relapses or for high-risk leukemias. There are two types of transplants: